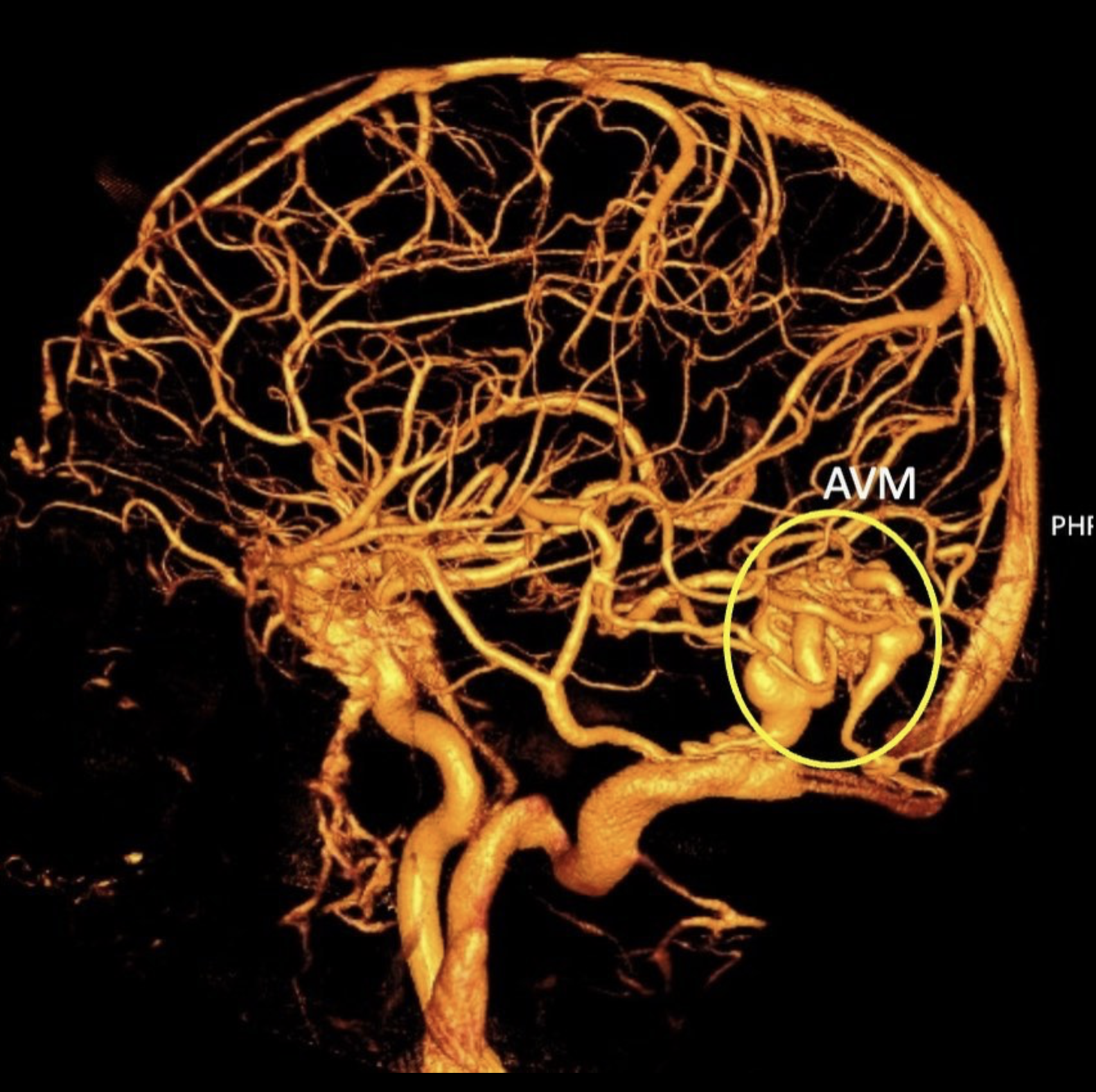
Arteriovenous Malformation (AVM)
Arteriovenous malformation (AVM) is a relatively rare but potentially dangerous condition that affects the blood vessels near the brain. Unlike cerebral aneurysms, which are characterized by blood vessel dilations, AVMs involve abnormal tangles of blood vessels. This condition, though accounting for only 3-5% of the population, can have severe implications for those affected. AVMs are more commonly found in women over the age of 30, further highlighting the need for awareness and timely diagnosis. This disparity may be attributed to hormonal factors, although the precise causes of AVMs remain largely unknown. One of the most concerning aspects of AVMs is their elusive nature. Many individuals live with AVMs, completely unaware of their presence until an event triggers symptoms. It is during these moments that the true danger of AVMs becomes evident, as they can rupture or cause significant damage to the surrounding brain tissue. When an AVM ruptures, it can lead to a hemorrhage, causing symptoms such as sudden severe headaches, seizures, neurologic deficits, or in some cases, even loss of consciousness. Early identification of AVMs is crucial in order to minimize the risk of life-threatening complications.
-
Arteriovenous malformations (AVMs) result from abnormal connections between arteries and veins in the brain or spinal cord. These formations occur during fetal development, and the exact cause is not well understood. However, there are several factors that may contribute to the development of AVMs. These include genetic predisposition, certain congenital conditions (such as hereditary hemorrhagic telangiectasia), and exposure to certain environmental factors (such as radiation). It is important to note that the majority of AVMs are sporadic and not inherited. While the specific cause of AVMs remains largely unknown, understanding the potential contributing factors can help healthcare professionals in diagnosing and treating these conditions.
-
Seizures and Neurological Signs of Brain Arteriovenous Malformation (AVM)Brain AVMs, or arteriovenous malformations, can present with various symptoms. These include:
Seizures
Headache or localized head pain
Muscle weakness or numbness affecting specific parts of the body
Furthermore, depending on the specific location of the AVM within the brain, more severe neurological signs and symptoms may arise. These can include:
Intense headaches
Weakness, numbness, or even paralysis of particular body regions
Vision loss
Difficulties with speech
Confusion or an inability to comprehend others
Severe unsteadiness or coordination issues
It is important to note that the onset of symptoms associated with brain AVMs can occur at any age. However, they commonly manifest between the ages of 10 and 40. Over time, these AVMs can gradually cause damage to the surrounding brain tissue. As a result, symptoms typically begin to manifest during early adulthood.
-
Diagnosing AVMs often involves the use of advanced imaging techniques, such as computed tomography (CT) or magnetic resonance imaging (MRI). These tests provide detailed images of the blood vessels, aiding in the accurate detection and characterization of the abnormality.
-
The selection of treatment depends on factors such as the size, location, and symptoms associated with the AVM. One approach is surgical resection, where a neurosurgeon removes the AVM through a craniotomy procedure. Another method is endovascular embolization, which involves the insertion of a catheter into the blood vessels to block the abnormal connections using glue or other embolic agents. Radiosurgery, using methods like stereotactic radiosurgery, is yet another treatment option. This non-invasive approach delivers precisely targeted radiation to the AVM, causing it to gradually close off over time. The choice of treatment depends on various factors, and a thorough evaluation by a neurosurgeon specializing in AVM management is crucial to determine the most appropriate course of action for each patient.