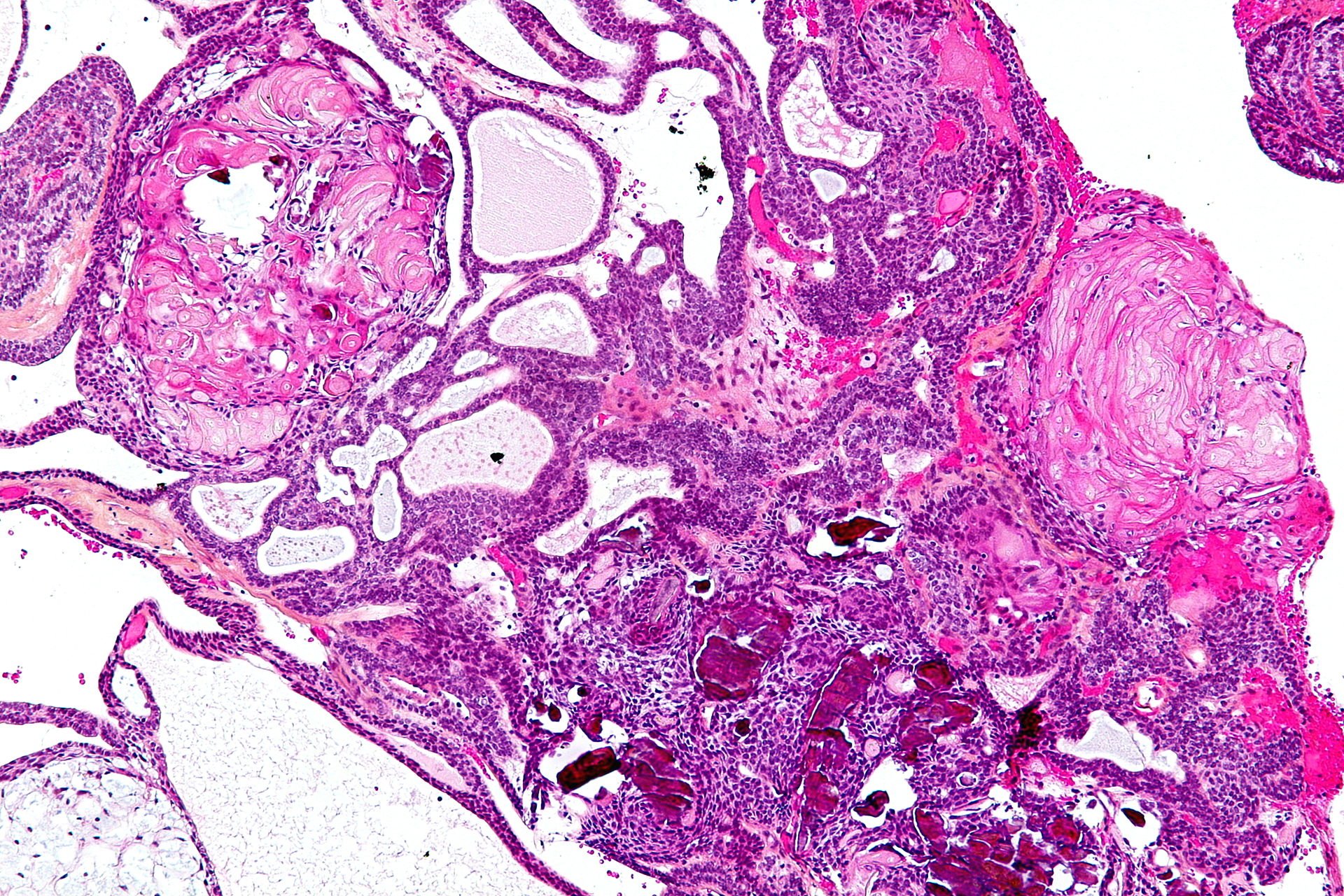
Craniopharyngiomas
Craniopharyngiomas are usually benign and do not produce hormones, and may present in various forms such as solid, cystic (containing fluid), or with debris and calcification or bone formation. Due to their slow growth, it may take years before symptoms become noticeable and a diagnosis is established. These tumors can be located either above (suprasellar) or within (intrasellar) the sella turcica and may result in varying degrees of hypopituitarism as they compress the anterior pituitary gland (adenohypophysis), pituitary stalk, or hypothalamus.
-
Craniopharyngiomas have a congenital origin, as they originate from the cricopharyngeal duct, which is the embryonic structure that connects the brain to the pharynx and through which the eventual adenohypophysis and infundibulum migrate. The name of the tumor, which combines the roots "Cranio" (skull), "pharynx" (throat), and "oma" (tumor), reflects this origin. However, the exact cause or trigger of the tumor growth is not yet known.
-
Craniopharyngioma patients may exhibit a wide range of symptoms, from being completely asymptomatic (incidentally discovered) to experiencing endocrine, visual, or psychological disorders. While some patients may remain asymptomatic for extended periods, others may experience a progressive deterioration in their clinical condition. The manifestation of symptoms in a craniopharyngioma patient is determined by the location and size of the tumor. Such symptoms may include an increase in intracranial pressure (ICP) due to obstruction of cerebrospinal fluid (CSF) pathways, leading to headaches, nausea, vomiting, and difficulty with balance. Additionally, direct pressure on the surrounding neurovascular structures may cause a decline in vision, especially peripheral vision, resulting from the tumor's compression on the optic nerves.
-
To diagnose a craniopharyngioma, the initial steps involve obtaining a detailed medical history and performing a neurological examination. After this, it is necessary to conduct a comprehensive radiological evaluation to determine the appropriate treatment approach and identify any tumors that may require multiple surgical procedures. This imaging evaluation typically involves both magnetic resonance imaging (MRI) and computed tomography (CT) scans, which are performed with and without intravenous contrast. Because craniopharyngiomas can cause vision and hormonal problems, patients are often given a baseline evaluation by an ophthalmologist and an endocrinologist.
-
Craniopharyngiomas have traditionally been treated with surgery as the primary treatment option. However, in some cases, radiation therapy (either conventional or gamma knife) and intra-tumoral chemotherapy may be appropriate. These treatments may be used alone or in combination, particularly in cases where residual tumor remains after surgery. In younger children, radiation and chemotherapy may be avoided to prevent potential long-term side effects.

